
Allergy Shots
Allergy shots are administered on a regular basis exposing the body to a little amount of an allergen to establish immunity.
learn moreAllergy, Asthma & Immunology of the Rockies has a Board-Certified Allergists and Immunologists closer than you think. Request an appointment in-person or by telemedicine today to get relief from allergies and asthma – and get back to living!
970-947-0600Schedule an appointment and get allergy and asthma relief.

Looking for a local asthma, allergy, or immunology specialist near you?
Our board-certified doctors understand unique allergy and asthma issues affecting those in and around the Roaring Fork and Eagle Valley. Call us today to schedule an appointment and start feeling your best!

Allergy Shots
Allergy shots are administered on a regular basis exposing the body to a little amount of an allergen to establish immunity.
learn more
Telemedicine
To help you and your family to be healthy wherever they are, you can access healthcare anywhere.
learn more
Biologics for Asthma
These are new, highly effective, medicines that help prevent moderate-to-severe asthma given once or twice a month.
learn more
Pulmonary Function Tests
These tests help your provider diagnose and monitor asthma symptoms by measuring your overall lung health.
learn more
Skin Allergy Testing
This is less invasive than blood tests and is a good alternative for patients who don’t like needles.
learn more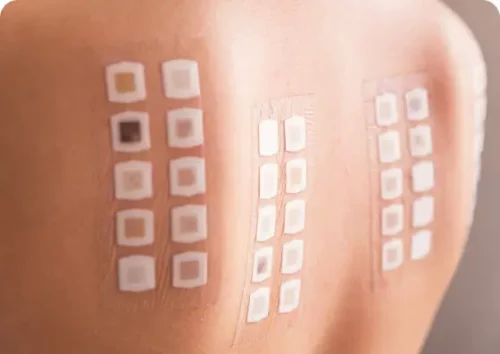
Allergy Patch Testing
Allergy patch testing is a common test used to confirm the cause of allergic contact dermatitis.
learn more
Food Allergy Testing
A challenge test is a highly accurate diagnostic test to determine if a patient has outgrown a food allergy.
learn more
Drug Allergy Testing
This involves gradually introducing the medication in small doses until the therapeutic dose is achieved.
learn moreOur team of experienced allergists and immunologists will work with you to create a personalized treatment plan that suits your needs and goals. Contact us today to schedule an appointment and start your journey to better health.
Since 2008, we have provided full-service allergy and asthma care to Summit County and Roaring Fork and Eagle Valley residents. We hope to provide patients with the best care possible with our compassionate staff, well-educated and experienced doctors, and cutting-edge medical equipment and therapies.
The doctors at Allergy, Asthma & Immunology of the Rockies are dedicated to improving quality of life, helping each patient that walks through their doors get back to enjoying the activities that make them happy — without worrying about allergies standing in their way.

Regan Pyle, DO is a board-certified Allergist/Immunologist who trained at Mayo Clinic in Rochester, MN. Prior to her fellowship, she completed medical school at Kansas City University and residency at the University of Louisville. She truly empathizes and understands that there’s often more to an allergy than the condition itself. That’s why she has a whole-patient approach to care by actively listening and engaging in discussion with her patients to create the best treatment plan for them. Dr. Pyle is thrilled to offer state of the art Allergy and Immunology care in the beautiful Rocky Mountains.
Make an AppointmentWe are dedicated to improving quality of life, helping each patient that walks through their doors get back to enjoying the activities that make them happy — without worrying about allergies standing in their way.
Make an Appointment
Change your life, and the lives of others
Achieve personal success and change lives when you work with us! Join a group of innovative physicians, experienced clinical staff, and administrative support teams who live every day on mission and wake up excited to tackle new challenges, striving to improve patients’ health and quality of life.
Allergy, Asthma & Immunology of the Rockies is part of the AllerVie Health network, a leading national network of allergy and asthma providers. All of our career opportunities are posted on AllerVie Health’s main Careers webpage.
Join our Team